Read the case history over the next few pages, detailing a likely scenario of a patient being investigated in the Haematology laboratory. Write a case study using the attached guidance. The word count is 2,500 (excluding tables, figures, legends and references). State your word count at the end of the case study.
A 28 year old woman was visited by her GP. She had been complaining of general malaise for some days, and now appeared flushed and was sweating. She had developed several bruises over her body without, apparently, any significant cause. She was very agitated.
On examination, her GP found that she had an oral temperature of 39.4o C, and a heartbeat of 115 beats a minute. Although flushed, her nails were pale, and she had widespread bruising. Examination of her oral cavity revealed ulceration, a gum infection and some gum bleeding. The GP arranged for her to be taken urgently for admission to hospital under the care of the consultant haematologist. In hospital, the patient had samples of blood taken for full blood count (FBC), clotting screen and for blood grouping.
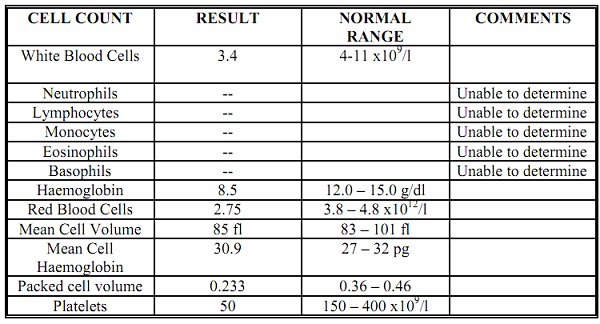
FBC results:
The sample for an FBC was processed on a Sysmex counter late afternoon, and produced the following results:
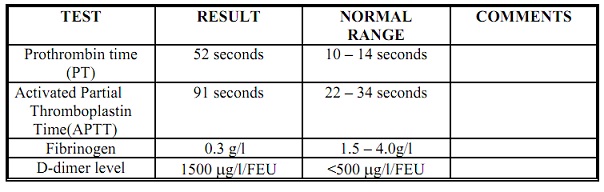
Clotting screen results:
These were performed while the FBC was being processed.
Blood film analysis:
A Biomedical Scientist made a blood film and stained it. She then examined the blood film and reported the following:-
Red cells showed varying cell shapes and sizes. Occasional nucleated red blood cells were seen. Occasional red cell fragments were seen. Marked thrombocytopaenia.
A manual differential white blood cell count was performed by this biomedical scientist, with the following results (overleaf):-
Neutrophils 2% of white cells
Lymphocytes 17% “
Monocytes 1% “
Myelocytes 19% “
Promyelocytes 59% “
Blast cells 2% “
The biomedical scientist contacted the consultant haematologist to let her know the results from the FBC and clotting tests. The consultant then came to the lab to scan the blood film herself and made the following blood film comments:–
Many promyelocytes seen with azurophilic granules and bundles of Auer rods.
Blood group test results:
She was found to be O Rhesus (D) positive, with no atypical antibodies present.
Initial treatment of patient:
The consultant haematologist contacted staff in the Blood Transfusion department, and requested that 1 unit of platelets, and 4 units of FFP be given that evening to the patient. Antibiotics (gentomycin and meropenem) were started too, along with ‘ATRA’.
Further investigative tests:
Bone marrow processing:
While waiting for the Blood Transfusion products to be ready, the consultant haematologist took a bone marrow sample from the patient. A bone marrow film was made, stained on the same evening, then examined the following morning by the consultant haematologist. She reported on the presence of:-
“many heavily granulated promyelocytes, with multiple Auer rods and bi-lobed nuclei”.
Bone marrow flow cytometry:
This was performed during the morning of day 2 on the original bone marrow sample taken.
The promyelocytes were:-
HLA-DR = negative,
CD13 positive,
CD33 positive.
The Genetics laboratory carried out a cytogenetics analysis of the bone marrow cells, revealing a translocation of part of chromosome 15 to chromosome 17.
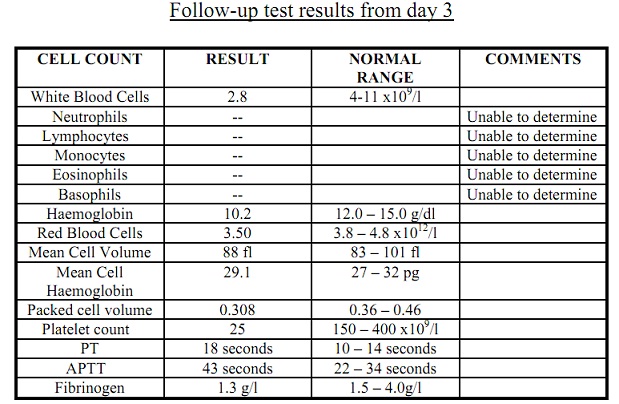
Follow-up test results and treatment for day 2
Repeat test results from day 2
The following results had changed significantly; Haemoglobin had fallen to 7.7 g/dl, PT had shortened to 30 seconds, and the APTT had shortened to 62 seconds.
Further treatment:
The consultant haematologist asked for the following products from the Blood Transfusion department:-
2 units of packed red cells,
1 unit of platelets,
4 units of FFP.
The patient was also started on chemotherapy.
Summary of further treatment:
Over the following week, the patient continued to receive ATRA, chemotherapy and antibiotics. Red cells, FFP and platelets were no longer given.
Guide to writing case studies:
In the laboratory, we produce thousands of test results every day. It can be easy to forget that each sample has a patient’s story behind it, in which the Haematology result that we see is often only the tip of the iceberg. Case studies are a good way of unraveling that story, and at the same time learning about a condition or disease in a different and
hopefully interesting way.
A case study is a standard format for recounting the story of a specific case. A case study should have the following format:
Case History:
Begin by describing the way in which the patient came to be seen by a doctor. Describe their symptoms, history and some haematological results. In cases where clinical details are elaborate, you may want to simplify them to ensure your audience can understand. You can use tables to present data.
Then go on to describe the haematological abnormalities and what they mean. Give the diagnosis and explain how this was decided upon – are there any other conditions which could give rise to the patient’s symptoms? How could the diagnosis be confirmed by other tests?
If the patient underwent any treatment, describe this. Why was this treatment selected?
Discussion:
Describe the disease itself – incidence, clinical features, likely progression, typical haematological presentation etc.
Describe the cause of the disease and any biochemical pathways involved. Why do the haematological abnormalities described occur?
Describe the treatment options available and the likely outcome for these patients.
Is there any research currently taking place in this field/are there any future developments likely?
Conclusion: Conclude your case study with a summary of what you have presented.
References:
You should use a variety of sources (aim for at least 10; in order to get a high mark one of the things you must show is that you have done plenty of reading and research around the subject) and use the Harvard method of citing and referencing work.
Learning how to use Harvard referencing properly is NOT time consuming, you may lose lots of marks if you reference incorrectly.
In the case study you should also address the following:
The patient appears to be anaemic, list the test results in the 1st FBC that relate to this, and explain how some of the patient’s symptoms can be attributed to them.
List which symptoms and test results in the 1st FBC/blood film analysis directly relate to the patient having infections, and explain why infections were likely in this patient.
Explain why the patient could have developed multiple bruises, and how laboratory tests from the initial investigative tests relate to this.